Cetuximab anaphylaxis and tick bites – a rare but important association for patients living in high tick prevalence areas.
Cetuximab anaphylaxis and tick bites – a rare but important association for patients living in high tick prevalence areas.
Alexander Yuile 1 2 3 , Claudia Fanuli 1 3 , Sheryl van Nunen 2 , Connie Diakos 1 2 3 , Stephen Clarke 1 2 3 , Christian Steiner 1 3 , Robyn MacMillan 1 3 , Meredith Oatley 2 , Nick Pavlakis 1 2 3
1. Medical Oncology, Northern Cancer Institute, St Leonards, NSW, Australia
2. Medical Oncology, Royal North Shore Hospital, St Leonards, NSW, Australia
3. Medical Oncology, Northern Cancer Institute, Frenchs Forrest, NSW, Australia
Dr Alexander Yuile Medical Oncology, Northern Cancer Institute, St Leonards, NSW, Australia has presented his review “Cetuximab anaphylaxis and tick bites – a rare but important association for patients living in high tick prevalence areas” at the Clinical Oncology Society of Australia 46th Annual Scientific Meeting.
This retrospective study reviews the experience of two community cancer centres in high tick exposure areas in Sydney with cetuximab anaphylaxis and proposes a protocol to avoid this.
Background
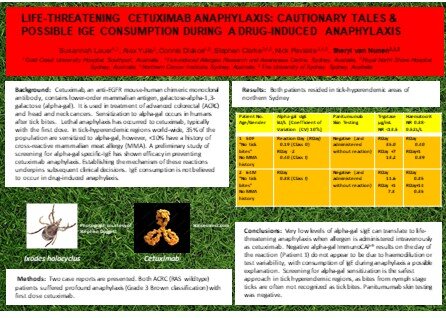
Cetuximab (cetux) is an anti-EGFR mouse-human chimeric monoclonal antibody used to treat advanced head and neck and colorectal cancers (CRC). Initial data suggested grade 4 cetux infusion reactions occurred in 1.7%, many on first exposure. The majority of those with anaphylactic reactions possess pre-developed IgE antibodies to galactose-alpha-1,3-galactose (alpha-gal). It is thought that the vector for pre-exposure to alpha-gal is antigen inoculation via tick bites. This retrospective study reviews the experience of two community cancer centres in high tick exposure areas in Sydney with cetux anaphylaxis and proposes a protocol to avoid this.
Method
The number of severe cetux infusions occurring in the Northern Cancer Institute Frenchs Forrest and St Leonards clinics, Sydney were recorded from May 2014 to February 2019. To capture anaphylaxis, patients requiring adrenaline were recorded.
Results
A total of 87 patients received cetux in this period. Seven patients (8.3%) experienced at least a grade 3 reaction, four females, age range 41-72 years (median 58.9 years). Three patients (3.5%) had a grade 4 reaction (requiring adrenaline) with confirmed anaphylaxis criteria. All three were receiving cetux for metastatic CRC and their anaphylaxis occurred with the first infusion. No patients had a documented or known history of mammalian meat allergy and all patients lived in Northern Sydney in areas with a high tick prevalence.
Conclusion
These cases support the existing theory of increased rates of cetux anaphylaxis in areas of high tick prevalence with the incidence twice that predicted in original studies. Based on this, we recommend the following protocol for patients considered for cetux therapy: Known mammalian meat allergy as an absolute contraindication; patients with a history of tick bites or living in a high tick prevalence area should have RAST (ImmunoCAP®) testing for alpha-gal specific-IgE-specific antibodies. Those who test positive should be given alternate therapy.